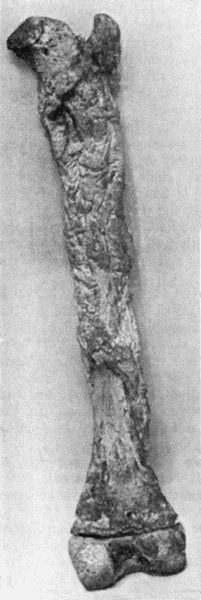
Fig. 118.—Shaft of Femur after Acute Osteomyelitis. The shaft has undergone extensive necrosis, and a shell of new bone has been formed by the periosteum.
Diseases caused by the Staphylococcus Aureus.—As the majority of pyogenic diseases are due to infection with the staphylococcus aureus, these will be described first.
Acute osteomyelitis is a suppurative process beginning in the marrow and tending to spread to the periosteum. The disease is common in children, but is rare after the skeleton has attained maturity. Boys are affected more often than girls, in the proportion of three to one, probably because they are more liable to exposure, to injury, and to violent exertion.
Etiology.—Staphylococci gain access to the blood-stream in various ways, it may be through the skin or through a mucous surface.
Such conditions as, for example, a blow, some extra exertion such as a long walk, or exposure to cold, as in wading, may act as localising factors.
The long bones are chiefly affected, and the commonest sites are: either end of the tibia and the lower end of the femur; the other bones of the skeleton are affected in rare instances.
Pathology.—The disease commences and is most intense in the marrow of the ossifying junction at one end of the diaphysis; it may commence at both ends simultaneously—bipolar osteomyelitis; or, commencing at one end, may spread to the other.
The changes observed are those of intense engorgement of the marrow, going on to greenish-yellow purulent infiltration. Where the process is most advanced—that is, at the ossifying junction—there are evidences of absorption of the framework of the bone; the marrow spaces and Haversian canals undergo enlargement and become filled with greenish-yellow pus. This rarefaction of the spongy bone is the earliest change seen with the X-rays.
The process may remain localised to the ossifying junction, but usually spreads along the medullary canal for a varying distance, and also extends to the periosteum by way of the enlarged Haversian canals. The pus accumulates under the periosteum and lifts it up from the bone. The extent of spread in the medullary canal and beneath the periosteum is in close correspondence. The periosteum of the diaphysis is easily separated—hence the facility with which the pus spreads along the shaft; but in the region of the ossifying junction it is raised with difficulty because of its intimate connection with the epiphysial cartilage. Less frequently there is more than one collection of pus under the periosteum, each being derived from a focus of suppuration in the subjacent marrow. The pus perforates the periosteum, and makes its way to the surface by the easiest anatomical route, and discharges externally, forming one or more sinuses through which fresh infection may take place. The infection may spread to the adjacent joint, either directly through the epiphysis and articular cartilage, or along the deep layer of the periosteum and its continuation—the capsular ligament. When the epiphysis is intra-articular, as, for example, in the head of the femur, the pus when it reaches the surface of the bone necessarily erupts directly into the joint.
While the occurrence of purely periosteal suppuration is regarded as possible, we are of opinion that the embolic form of staphylococcal osteomyelitis always originates in the marrow.
The portion of the diaphysis which has sustained the action of the concentrated toxins has its vitality further impaired as a result of the stripping of the periosteum and thrombosis of the blood vessels of the marrow, so that necrosis of bone is one of the most striking results of the disease, and as this takes place rapidly, that is, in a day or two, the term acute necrosis, formerly applied to the disease, was amply justified.
When there is marked rarefaction of the bone at the ossifying junction, the epiphysis is liable to be separated—epiphysiolysis. The separation usually takes place through the young bone of the ossifying junction, and the surfaces of the diaphysis and epiphysis are opposed to each other by irregular eroded surfaces bathed in pus. The separated epiphysis may be kept in place by the periosteum, but when this has been detached by the formation of pus beneath it, the epiphysis is liable to be displaced by muscular action or by some movement of the limb, or it is the diaphysis that is displaced, for example, the lower end of the diaphysis of the femur may be projected into the popliteal space.
The epiphysial cartilage usually continues its bone-forming functions, but when it has been seriously damaged or displaced, the further growth of the bone in length may be interfered with. Sometimes the separated and displaced epiphysis dies and constitutes a sequestrum.
The adjacent joint may become filled at an early stage with a serous effusion, which may be sterile. When the cocci gain access to the joint, the lesion assumes the characters of a purulent arthritis, which, from its frequency during the earlier years of life, has been called the acute arthritis of infants.
Separation of an epiphysis nearly always results in infection and destruction of the adjacent joint.
Osteomyelitis is rare in the bones of the carpus and tarsus, and the associated joints are usually infected from the outset. In flat bones, such as the skull, the scapula, or the ilium, suppuration usually occurs on both aspects of the bone as well as in the marrow.
Clinical Features.—The constitutional symptoms, which are due to the associated toxæmia, vary considerably in different cases. In mild cases they may be so slight as to escape recognition. In exceptionally severe cases the patient may succumb before there are obvious signs of the localisation of the staphylococci in the bone marrow. In average cases the temperature rises rapidly with a rigor and runs an irregular course with morning remissions, there is marked general illness accompanied by headache, vomiting, and sometimes delirium.
The local manifestations are pain and tenderness in relation to one of the long bones; the pain may be so severe as to prevent sleep and to cause the child to cry out. Tenderness on pressure over the bone is the most valuable diagnostic sign. At a later stage there is an ill-defined swelling in the region of the ossifying junction, with œdema of the overlying skin and dilatation of the superficial veins.
The swelling appears earlier and is more definite in superficial bones such as the tibia, than in those more deeply placed such as the upper end of the femur. It may be less evident to the eye than to the fingers, and is best appreciated by gently stroking the bone from the middle of its shaft towards the end. The maximum thickening and tenderness usually correspond to the junction of the diaphysis with the epiphysis, and the swelling tails off gradually along the shaft. As time goes on there is redness of the skin, especially over a superficial bone, such as the tibia, the swelling becomes softer, and gives evidence of fluctuation. This stage may be reached at the end of twenty-four hours, or not for some days.
Suppuration spreads towards the surface, until, some days later, the skin sloughs and pus escapes, after which the fever usually remits and the pain and other symptoms are relieved. The pus may contain blood and droplets of fat derived from the marrow, and in some cases minute particles of bone are present also. The presence of fat and bony particles in the pus confirms the medullary origin of the suppuration.
If an incision is made, the periosteum is found to be raised from the bone; the extent of the bare bone will be found to correspond fairly accurately with the extent of the lesion in the marrow.
Local Complications.—The adjacent joint may exhibit symptoms which vary from those of a simple effusion to those of a purulent arthritis. The joint symptoms may count for little in the clinical picture, or, as in the case of the hip, may so predominate as to overshadow those of the bone lesion from which they originated.
Separation and displacement of the epiphysis usually reveals itself by an alteration in the attitude of the limb; it is nearly always associated with suppuration in the adjacent joint.
When pathological fracture of the shaft occurs, as it may do, from some muscular effort or strain, it is attended with the usual signs of fracture.
Dislocation of the adjacent joint has been chiefly observed at the hip; it may result from effusion into the joint and stretching of the ligaments, or may be the sequel of a purulent arthritis; the signs of dislocation are not so obvious as might be expected, but it is attended with an alteration in the attitude of the limb, and the displacement of the head of the bone is readily shown in a skiagram.
General Complications.—In some cases a multiplicity of lesions in the bones and joints imparts to the disease the features of pyæmia. The occurrence of endocarditis, as indicated by alterations in the heart sounds and the development of murmurs, may cause widespread infective embolism, and metastatic suppurations in the kidneys, heart-wall, and lungs, as well as in other bones and joints than those primarily affected. The secondary suppurations are liable to be overlooked unless sought for, as they are rarely attended with much pain.
In these multiple forms of osteomyelitis the toxæmic symptoms predominate; the patient is dull and listless, or he may be restless and talkative, or actually delirious. The tongue is dry and coated, the lips and teeth are covered with sordes, the motions are loose and offensive, and may be passed involuntarily. The temperature is remittent and irregular, the pulse small and rapid, and the urine may contain blood and albumen. Sometimes the skin shows erythematous and purpuric rashes, and the patient may cry out as in meningitis. The post-mortem appearances are those of pyæmia.
Differential Diagnosis.—Acute osteomyelitis is to be diagnosed from infections of the soft parts, such as erysipelas and cellulitis, and, in the case of the tibia, from erythema nodosum. Tenderness localised to the ossifying junction is the most valuable diagnostic sign of osteomyelitis.
When there is early and pronounced general intoxication, there is likely to be confusion with other acute febrile illnesses, such as scarlet fever. In all febrile conditions in children and adolescents, the ossifying junctions of the long bones should be examined for areas of pain and tenderness.
Osteomyelitis has many features in common with acute articular rheumatism, and some authorities believe them to be different forms of the same disease (Kocher). In acute rheumatism, however, the joint symptoms predominate, there is an absence of suppuration, and the pains and temperature yield to salicylates.
The prognosis varies with the type of the disease, with its location—the vertebræ, skull, pelvis, and lower jaw being specially unfavourable—with the multiplicity of the lesions, and with the development of endocarditis and internal metastases.
Treatment.—This is carried out on the same lines as in other pyogenic infections.
In the earliest stages of the disease, the induction of hyperæmia is indicated, and should be employed until the diagnosis is definitely established, and in the meantime preparations for operation should be made. An incision is made down to and through the periosteum, and whether pus is found or not, the bone should be opened in the vicinity of the ossifying junction by means of a drill, gouge, or trephine. If pus is found, the opening in the bone is extended along the shaft as far as the periosteum has been separated, and the infected marrow is removed with the spoon. The cavity is then lightly packed with rubber dam, or, as recommended by Bier, the skin edges are brought together by sutures which are loosely tied to afford sufficient space between them for the exit of discharge, and the hyperæmic treatment is continued.
When there is widespread suppuration in the marrow, and the shaft is extensively bared of periosteum and appears likely to die, it may be resected straight away or after an interval of a day or two. Early resection of the shaft is also indicated if the opening of the medullary canal is not followed by relief of symptoms. In the leg and forearm, the unaffected bone maintains the length and contour of the limb; in the case of the femur and humerus, extension with weight and pulley along with some form of moulded gutter splint is employed with a similar object.
Amputation of the limb is reserved for grave cases, in which life is endangered by toxæmia, which is attributed to the primary lesion. It may be called for later if the limb is likely to be useless, as, for example, when the whole shaft of the bone is dead without the formation of a new case, when the epiphyses are separated and displaced, and the joints are disorganised.
Flat bones, such as the skull or ilium, must be trephined and the pus cleared out from both aspects of the bone. In the vertebræ, operative interference is usually restricted to opening and draining the associated abscess.
Nature's Effort at Repair.—In cases which are left to nature, and in which necrosis of bone has occurred, those portions of the periosteum and marrow which have retained their vitality resume their osteogenetic functions, often to an exaggerated degree. Where the periosteum has been lifted up by an accumulation of pus, or is in contact with bone that is dead, it proceeds to form new bone with great activity, so that the dead shaft becomes surrounded by a sheath or case of new bone, known as the involucrum (Fig. 118). Where the periosteum has been perforated by pus making its way to the surface, there are defects or holes in the involucrum, called cloacæ. As these correspond more or less in position to the sinuses in the skin, in passing a probe down one of the sinuses it usually passes through a cloaca and strikes the dead bone lying in the interior. If the periosteum has been extensively destroyed, new bone may only be formed in patches, or not at all. The dead bone is separated from the living by the agency of granulation tissue with its usual complements of phagocytes and osteoclasts, so that the sequestrum presents along its margins and on its deep surface a pitted, grooved, and worm-eaten appearance, except on the periosteal aspect, which is unaltered. Ultimately the dead bone becomes loose and lies in a cavity a little larger than itself; the wall of the cavity is formed by the new case, lined with granulation tissue. The separation of the sequestrum takes place more rapidly in the spongy bone of the ossifying junction than in the compact bone of the shaft.
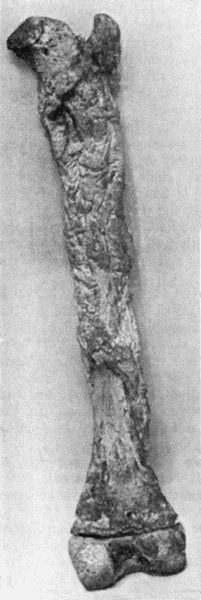
Fig. 118.—Shaft of Femur after Acute Osteomyelitis. The shaft has undergone extensive necrosis, and a shell of new bone has been formed by the periosteum.
When foci of suppuration have been scattered up and down the medullary cavity, and the bone has died in patches, several sequestra may be included by the new case; each portion of dead bone is slowly separated, and comes to lie in a cavity lined by granulations.
Even at a distance from the actual necrosis there is formation of new bone by the marrow; the medullary canal is often obliterated, and the bone becomes heavier and denser—sclerosis; and the new bone which is deposited on the original shaft results in an increase in the girth of the bone—hyperostosis.
Pathological fracture of the shaft may occur at the site of necrosis, when the new case is incapable of resisting the strain put upon it, and is most frequently met with in the shaft of the femur. Short of fracture, there may be bending or curving of the new case, and this results in deformity and shortening of the limb (Fig. 119).
The extrusion of a sequestrum may occur, provided there is a cloaca large enough to allow of its escape, but the surgeon has usually to interfere by performing the operation of sequestrectomy. Displacement or partial extrusion of the dead bone may cause complications, as when a sequestrum derived from the trigone of the femur perforates the popliteal artery or the cavity of the knee-joint, or a sequestrum of the pelvis perforates the wall of the urinary bladder.
The extent to which bone which has been lost is reproduced varies in different parts of the skeleton: while the long bones, the scapula, the mandible, and other bones which are developed in cartilage are almost completely re-formed, bones which are entirely developed in membrane, such as the flat bones of the skull and the maxilla, are not reproduced.
It may be instructive to describe the X-ray appearances of a long bone that has passed through an attack of acute osteomyelitis severe enough to have caused necrosis of part of the diaphysis. The shadow of the dead bone is seen in the position of the original shaft which it represents; it is of the same shape and density as the original shaft, while its margins present an irregular contour from the erosion concerned in its separation. The sequestrum is separated from the living bone by a clear zone which corresponds to the layer of granulations lining the cavity in which it lies. This clear zone separating the shadow of the dead bone from that of the living bone by which it is surrounded is conclusive evidence of a sequestrum. The medullary canal in the vicinity of the sequestrum being obliterated, is represented by a shadow of varying density, continuous with that of the surrounding bone. The shadow of the new case or involucrum with its wavy contour is also in evidence, with its openings or cloacæ, and is mainly responsible for the increase in the diameter of the bone.
The skiagram may also show separation and displacement of the adjacent epiphysis and destruction of the articular surfaces or dislocation of the joint.
Sequelæ of Acute Suppurative Osteomyelitis.—The commonest sequel is the presence of a sequestrum with one or more discharging sinuses; owing to the abundant formation of scar tissue these sinuses have rigid edges which are usually depressed and adherent to the bone.

Fig. 119.—Femur and Tibia showing results of Acute Osteomyelitis affecting Trigone of Femur; sequestrum partly surrounded by new case; backward displacement of lower epiphysis and implication of knee-joint.
The Recognition and Removal of Sequestra.—So long as there is dead bone there will be suppuration from the granulations lining the cavity in which it lies, and a discharge of pus from the sinuses, so that the mere persistence of discharge after an attack of osteomyelitis, is presumptive evidence of the occurrence of necrosis. Where there are one or more sinuses, the passage of a probe which strikes bare bone affords corroboration of the view that the bone has perished. When the dead bone has been separated from the living, the X-rays yield the most exact information.
The traditional practice is to wait until the dead bone is entirely separated before undertaking an operation for its removal, from fear, on the one hand, of leaving portions behind which may keep up the discharge, and, on the other, of removing more bone than is necessary. This practice need not be adhered to, as by operating at an earlier stage healing is greatly hastened. If it is decided to wait for separation of the dead bone, drainage should be improved, and the infective element combated by the induction of hyperæmia.
The operation for the removal of the dead bone (sequestrectomy) consists in opening up the periosteum and the new case sufficiently to allow of the removal of all the dead bone, including the most minute sequestra. The limb having been rendered bloodless, existing sinuses are enlarged, but if these are inconveniently situated—for example, in the centre of the popliteal space in necrosis of the femoral trigone—it is better to make a fresh wound down to the bone on that aspect of the limb which affords best access, and which entails the least injury of the soft parts. The periosteum, which is thick and easily separable, is raised from the new case with an elevator, and with the chisel or gouge enough of the new bone is taken away to allow of the removal of the sequestrum. Care must be taken not to leave behind any fragment of dead bone, as this will interfere with healing, and may determine a relapse of suppuration.
The dead bone having been removed, the lining granulations are scraped away with a spoon, and the cavity is disinfected.
There are different ways of dealing with a bone cavity. It may be packed with gauze (impregnated with “bipp” or with iodoform), which is changed at intervals until healing takes place from the bottom; it may be filled with a flap of bone and periosteum raised from the vicinity, or with bone grafts; or the wall of bone on one side of the cavity may be chiselled through at its base, so that it can be brought into contact with the opposite wall. The method of filling bone cavities devised by Mosetig-Moorhof, consists in disinfecting and drying the cavity by a current of hot air, and filling it with a mixture of powdered iodoform (60 parts) and oil of sesame and spermaceti (each 40 parts), which is fluid at a temperature of 112° F.; the soft parts are then brought together without drainage. As the cavity fills up with new bone the iodoform is gradually absorbed. Iodoform gives a dark shadow with the X-rays, so that the process of its absorption can be followed in skiagrams taken at intervals.
These procedures may be carried out at the same time as the sequestrum is removed, or after an interval. In all of them, asepsis is essential for success.
The deformities resulting from osteomyelitis are more marked the earlier in life the disease occurs. Even under favourable conditions, and with the continuous effort at reconstruction of the bone by Nature's method, the return to normal is often far from perfect, and there usually remains a variable amount of hyperostosis and sclerosis and sometimes curving of the bone. Under less favourable conditions, the late results of osteomyelitis may be more serious. Shortening is not uncommon from interference with growth at the ossifying junction. Exaggerated growth in the length of a bone is rare, and has been observed chiefly in the bones of the leg. Where there are two parallel bones—as in the leg, for example—the growth of the diseased bone may be impaired, and the other continuing its normal growth becomes disproportionately long; less frequently the growth of the diseased bone is exaggerated, and it becomes the longer of the two. In either case, the longer bone becomes curved. An obliquity of the bone may result when one half of the epiphysial cartilage is destroyed and the other half continues to form bone, giving rise to such deformities as knock-knee and club-hand.
Deformity may also result from vicious union of a pathological fracture, permanent displacement of an epiphysis, contracture, ankylosis, or dislocation of the adjacent joint.
Relapsing Osteomyelitis.—As the term indicates, the various forms of relapsing osteomyelitis date back to an antecedent attack, and their occurrence depends on the capacity of staphylococci to lie latent in the marrow.
Relapse may take place within a few months of the original attack, or not for many years. Cases are sometimes met with in which relapses recur at regular intervals for several years, the tendency, however, being for the attacks to become milder as the virulence of the organisms becomes more and more attenuated.
Clinical Features.—Osteomyelitis in a patient over twenty-five is nearly always of the relapsing variety. In some cases the bone becomes enlarged, with pain and tenderness on pressure; in others there are the usual phenomena which attend suppuration, but the pus is slow in coming to the surface, and the constitutional symptoms are slight. The pus may escape by new channels, or one of the old sinuses may re-open. Radiograms usually furnish useful information as to the condition of the bone, both as it is altered by the original attack and by the changes that attend the relapse of the infective process.
Treatment.—In cases of thickening of the bone with persistent and severe pain, if relief is not afforded by the repeated application of blisters, the thickened periosteum should be incised, and the bone opened up with the chisel or trephine. In cases attended with suppuration, the swelling is incised and drained, and if there is a sequestrum, it must be removed.
Circumscribed Abscess of Bone—“Brodie's Abscess.”—The most important form of relapsing osteomyelitis is the circumscribed abscess of bone first described by Benjamin Brodie. It is usually met with in young adults, but we have met with it in patients over fifty. Several years may intervene between the original attack of osteomyelitis and the onset of symptoms of abscess.
Morbid Anatomy.[7]—The abscess is nearly always situated in the central axis of the bone in the region of the ossifying junction, although cases are occasionally met with in which it lies nearer the middle of the shaft. In exceptional cases there is more than one abscess (Fig. 120). The tibia is the bone most commonly affected, but the lower end of the femur, or either end of the humerus, may be the seat of the abscess. In the quiescent stage the lesion is represented by a small cavity in the bone, filled with clear serum, and lined by a fibrous membrane which is engaged in forming bone. Around the cavity the bone is sclerosed, and the medullary canal is obliterated. When the infection becomes active, the contents of the cavity are transformed into a greenish-yellow pus from which the staphylococcus can be isolated, and the cavity is lined by a thin film of granulation tissue which erodes the surrounding bone and so causes the abscess to increase in size. If the erosion proceeds uniformly, the cavity is spherical or oval; if it is more active at some points than others, diverticula or tunnels are formed, and one of these may finally erupt through the shell of the bone or into an adjacent joint. Small irregular sequestra are occasionally found within the abscess cavity. In long-standing cases it is common to find extensive obliteration of the medullary canal, and a considerable increase in the girth of the bone.
[7] Alexis Thomson, Edin. Med. Journ., 1906.
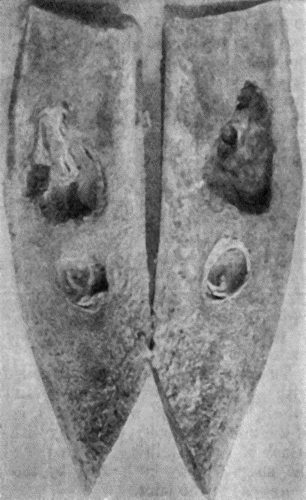
Fig. 120.—Segment of Tibia resected for Brodie's Abscess. The specimen shows two separate abscesses in the centre of the shaft, the lower one quiescent, the upper one active and increasing in size.
The size of the abscess ranges from that of a cherry to that of a walnut, but specimens in museums show that, if left to Nature, the abscess may attain much greater dimensions.
The affected bone is not only thicker and heavier than normal, but may also be curved or otherwise deformed as a result of the original attack of osteomyelitis.
The clinical features are almost exclusively local. Pain, due to tension within the abscess, is the dominant symptom. At first it is vague and difficult to localise, later it is referred to the interior of the bone, and is described as “boring.” It is aggravated by use of the limb, and there are often, especially during the night, exacerbations in which the pain becomes excruciating. In the early stages there are periods of days or weeks during which the symptoms abate, but as the abscess increases these become shorter, until the patient is hardly ever free from pain. Localised tenderness can almost always be elicited by percussion, or by compressing the bone between the fingers and thumb. The pain induced by the traction of muscles attached to the bone, or by the weight of the body, may interfere with the function of the limb, and in the lower extremity cause a limp in walking. The limb may be disabled from involvement of the adjacent joint, in which there may be an intermittent hydrops which comes and goes coincidently with exacerbations of pain; or the abscess may perforate the joint and set up an acute arthritis.
The diagnosis of Brodie's abscess from other affections met with at the ends of long bones, and particularly from tuberculosis, syphilis, and new growths, is made by a consideration of the previous history, especially with reference to an antecedent attack of osteomyelitis. When the adjacent joint is implicated, the surgeon may be misled by the patient referring all the symptoms to the joint.
The X-ray picture is usually diagnostic chiefly because all the lesions which are liable to be confused with Brodie's abscess—gumma, tubercle, myeloma, chondroma, and sarcoma—give a well-marked central clear area; the sclerosis around Brodie's abscess gives a dense shadow in which the central clear area is either not seen at all or only faintly (Fig. 121).
Treatment.—If an abscess is suspected, there should be no hesitation in exploring the interior of the bone. It is exposed by a suitable incision; the periosteum is reflected and the bone is opened up by a trephine or chisel, and the presence of an abscess may be at once indicated by the escape of pus. If, owing to the small size of the abscess or the density of the bone surrounding it, the pus is not reached by this procedure, the bone should be drilled in different directions.
Other Forms of Acute Osteomyelitis.—Among the less severe forms of osteomyelitis resulting from the action of attenuated organisms are the serous variety, in which an effusion of serous fluid forms under the periosteum; and growth fever, in which the child complains of vague evanescent pains (growing pains), and of feeling tired and disinclined to play; there may be some rise of temperature in the evening.
Infection with the staphylococcus albus, the streptococcus, or the pneumococcus also causes a mild form of osteomyelitis which may go on to suppuration.
Necrosis without suppuration, described by Paget under the name “quiet necrosis,” is a rare disease, and would appear to be associated with an attenuated form of staphylococcal infection (Tavel). It occurs in adults, being met with up to the age of fifty or sixty, and is characterised by the insidious development of a swelling which involves a considerable extent of a long bone. The pain varies in intensity, and may be continuous or intermittent, and there is tenderness on pressure. The shaft is increased in girth as a result of its being surrounded by a new case of bone. The resemblance to sarcoma may be very close, but the swelling is not as defined as in sarcoma, nor does it ever assume the characteristic “leg of mutton” shape. In both diseases there is a tendency to pathological fracture. It is difficult also in the absence of skiagrams to differentiate the condition from syphilitic and from tuberculous disease. If the diagnosis is not established after examination with the X-rays, an exploratory incision should be made; if dead bone is found, it is removed.
In typhoid fever the bone marrow is liable to be invaded by the typhoid bacillus, which may set up osteomyelitis soon after its lodgment, or it may lie latent for a considerable period before doing so. The lesions may be single or multiple, they involve the marrow or the periosteum or both, and they may or may not be attended with suppuration. They are most commonly met with in the tibia and in the ribs at the costo-chondral junctions.
The bone lesions usually occur during the seventh or eighth week of the fever, but have been known to occur much later. The chief complaint is of vague pains, at first referred to several bones, later becoming localised in one; they are aggravated by movement, or by handling the bone, and are worst at night. There is redness and œdema of the overlying soft parts, and swelling with vague fluctuation, and on incision there escapes a yellow creamy pus, or a brown syrupy fluid containing the typhoid bacillus in pure culture. Necrosis is exceptional.
When the abscess develops slowly, the condition resembles tuberculous disease, from which it may be diagnosed by the history of typhoid fever, and by obtaining a positive Widal reaction.
The prognosis is favourable, but recovery is apt to be slow, and relapse is not uncommon.
It is usually sufficient to incise the periosteum, but when the disease occurs in a rib it may be necessary to resect a portion of bone.
Pyogenic Osteomyelitis due to Spread of Infection from the Soft Parts.—There still remain those forms of osteomyelitis which result from infection through a wound involving the bone—for example, compound fractures, gun-shot injuries, osteotomies, amputations, resections, or operations for un-united fracture. In all of these the marrow is exposed to infection by such organisms as are present in the wound. A similar form of osteomyelitis may occur apart from a wound—for example, infection may spread to the jaws from lesions of the mouth; to the skull, from lesions of the scalp or of the cranial bones themselves—such as a syphilitic gumma or a sarcoma which has fungated externally; or to the petrous temporal, from suppuration in the middle ear.
The most common is an osteomyelitis commencing in the marrow exposed in a wound infected with pyogenic organisms. In amputation stumps, fungating granulations protrude from the sawn end of the bone, and if necrosis takes place, the sequestrum is annular, affecting the cross-section of the bone at the saw-line; or tubular, extending up the shaft, and tapering off above. The periosteum is more easily detached, is thicker than normal, and is actively engaged in forming bone. In the macerated specimen, the new bone presents a characteristic coral-like appearance, and may be perforated by cloacæ (Fig. 122).

Fig. 123.—New Periosteal Bone on surface of Femur from Amputation Stump. Osteomyelitis supervened on the amputation, and resulted in necrosis at the sawn section of the bone.
(Anatomical Museum, University of Edinburgh.)
Like other pyogenic infections, it may terminate in pyæmia, as a result of septic phlebitis in the marrow.
The clinical features of osteomyelitis in an amputation stump are those of ordinary pyogenic infection; the involvement of the bone may be suspected from the clinical course, the absence of improvement from measures directed towards overcoming the sepsis in the soft parts, and the persistence of suppuration in spite of free drainage, but it is not recognised unless the bone is exposed by opening up the stump or the changes in the bone are shown by the X-rays. The first change is due to the deposit of new bone on the periosteal surface; later, there is the shadow of the sequestrum.
Healing does not take place until the sequestrum is extruded or removed by operation.
In compound fractures, if a fragment dies and forms a sequestrum, it is apt to be walled in by new bone; the sinuses continue to discharge until the sequestrum is removed. Even after healing has taken place, relapse is liable to occur, especially in gun-shot injuries. Months or years afterwards, the bone may become painful and tender. The symptoms may subside under rest and elevation of the limb and the application of a compress, or an abscess forms and bursts with comparatively little suffering. The contents may be clear yellow serum or watery pus; sometimes a small spicule of bone is discharged. Valuable information, both for diagnosis and treatment, is afforded by skiagrams.