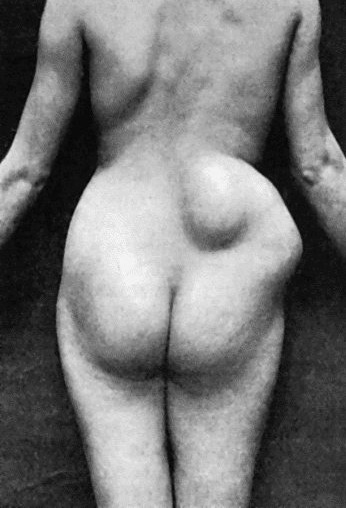
Fig. 34.—Tuberculous Abscess in right lumbar region in a woman aged thirty.
The caseation of tuberculous granulation tissue and its liquefaction is a slow and insidious process, and is unattended with the classical signs of inflammation—hence the terms “cold” and “chronic” applied to the tuberculous abscess.
In a cold abscess, such as that which results from tuberculous disease of the vertebræ, the clinical appearances are those of a soft, fluid swelling without heat, redness, pain, or fever. When toxic symptoms are present, they are usually due to a mixed infection.
A tuberculous abscess results from the disintegration and liquefaction of tuberculous granulation tissue which has undergone caseation. Fluid and cells from the adjacent blood vessels exude into the cavity, and lead to variations in the character of its contents. In some cases the contents consist of a clear amber-coloured fluid, in which are suspended fragments of caseated tissue; in others, of a white material like cream-cheese. From the addition of a sufficient number of leucocytes, the contents may resemble the pus of an ordinary abscess.
The wall of the abscess is lined with tuberculous granulation tissue, the inner layers of which are undergoing caseation and disintegration, and present a shreddy appearance; the outer layers consist of tuberculous tissue which has not yet undergone caseation. The abscess tends to increase in size by progressive liquefaction of the inner layers, caseation of the outer layers, and the further invasion of the surrounding tissues by tubercle bacilli. In this way a tuberculous abscess is capable of indefinite extension and increase in size until it reaches a free surface and ruptures externally. The direction in which it spreads is influenced by the anatomical arrangement of the tissues, and possibly to some extent by gravity, and the abscess may reach the surface at a considerable distance from its seat of origin. The best illustration of this is seen in the psoas abscess, which may originate in the dorsal vertebræ, extend downwards within the sheath of the psoas muscle, and finally appear in the thigh.
Clinical Features.—The insidious development of the tuberculous abscess is one of its characteristic features. The swelling may attain a considerable size without the patient being aware of its existence, and, as a matter of fact, it is often discovered accidentally. The absence of toxæmia is to be associated with the incapacity of the wall of the abscess to permit of absorption; this is shown also by the fact that when even a large quantity of iodoform is inserted into the cavity of the abscess, there are no symptoms of poisoning. The abscess varies in size from a small cherry to a cavity containing several pints of pus. Its shape also varies; it is usually that of a flattened sphere, but it may present pockets or burrows running in various directions. Sometimes it is hour-glass or dumb-bell shaped, as is well illustrated in the region of the groin in disease of the spine or pelvis, where there may be a large sac occupying the venter ilii, and a smaller one in the thigh, the two communicating by a narrow channel under Poupart's ligament. By pressing with the fingers the pus may be displaced from one compartment to the other. The usual course of events is that the abscess progresses slowly, and finally reaches a free surface—generally the skin. As it does so there may be some pain, redness, and local elevation of temperature. Fluctuation becomes evident and superficial, and the skin becomes livid and finally gives way. If the case is left to nature, the discharge of pus continues, and the track opening on the skin remains as a sinus. The persistence of suppuration is due to the presence in the wall of the abscess and of the sinus, of tuberculous granulation tissue, which, so long as it remains, continues to furnish discharge, and so prevents healing. Sooner or later pyogenic organisms gain access to the sinus, and through it to the wall of the abscess. They tend further to depress the resisting power of the tissues, and thereby aggravate and perpetuate the tuberculous disease. This superadded infection with pyogenic organisms exposes the patient to the further risks of septic intoxication, especially in the form of hectic fever and septicæmia, and increases the liability to general tuberculosis, and to waxy degeneration of the internal organs. The mixed infection is chiefly responsible for the pyrexia, sweating, and emaciation which the laity associate with consumptive disease. A tuberculous abscess may in one or other of these ways be a cause of death.
Residual abscess is the name given to an abscess that makes its appearance months, or even years, after the apparent cure of tuberculous disease—as, for example, in the hip-joint or spine. It is called residual because it has its origin in the remains of the original disease.
Diagnosis.—A cold abscess is to be diagnosed from a syphilitic gumma, a cyst, and from lipoma and other soft tumours. The differential diagnosis of these affections will be considered later; it is often made easier by recognising the presence of a lesion that is likely to cause a cold abscess, such as tuberculous disease of the spine or of the sacro-iliac joint. When it is about to burst externally, it may be difficult to distinguish a tuberculous abscess from one due to infection with pyogenic organisms. Even when the abscess is opened, the appearances of the pus may not supply the desired information, and it may be necessary to submit it to bacteriological examination. When the pus is found to be sterile, it is usually safe to assume that the condition is tuberculous, as in other forms of suppuration the causative organisms can usually be recognised. Experimental inoculation will establish a definite diagnosis, but it implies a delay of two to three weeks.
Treatment.—The tuberculous abscess may recede and disappear under general treatment. Many surgeons advise that so long as the abscess is quiescent it should be left alone. All agree, however, that if it shows a tendency to spread, to increase in size, or to approach the skin or a mucous membrane, something should be done to avoid the danger of its bursting and becoming infected with pyogenic organisms. Simple evacuation of the abscess by a hollow needle may suffice, or bismuth or iodoform may be introduced after withdrawal of the contents.
Evacuation of the Abscess and Injection of iodoform.—The iodoform is employed in the form of a 10 per cent. solution in ether or the same proportion suspended in glycerin. Either form becomes sterile soon after it is prepared. Its curative effects would appear to depend upon the liberation of iodine, which restrains the activity of the bacilli, and upon its capacity for irritating the tissues and so inducing a protective leucocytosis, and also of stimulating the formation of scar tissue. An anæsthetic is rarely called for, except in children. The abscess is first evacuated by means of a large trocar and cannula introduced obliquely through the overlying soft parts, avoiding any part where the skin is thin or red. If the cannula becomes blocked with caseous material, it may be cleared with a probe, or a small quantity of saline solution is forced in by the syringe. The iodoform is injected by means of a glass-barrelled syringe, which is firmly screwed on to the cannula. The amount injected varies with the size of the abscess and the age of the patient; it may be said to range from two or three drams in the case of children to several ounces in large abscesses in adults. The cannula is withdrawn, the puncture is closed by a Michel's clip, and a dressing applied so as to exert a certain amount of compression. If the abscess fills up again, the procedure should be repeated; in doing so, the contents show the coloration due to liberated iodine. When the contents are semi-solid, and cannot be withdrawn even through a large cannula, an incision must be made, and, after the cavity has been emptied, the iodoform is introduced through a short rubber tube attached to the syringe. Experience has shown that even large abscesses, such as those associated with spinal disease, may be cured by iodoform injection, and this even when rupture of the abscess on the skin surface has appeared to be imminent.
Another method of treatment which is less popular now than it used to be, and which is chiefly applicable in abscesses of moderate size, is by incision of the abscess and removal of the tuberculous tissue in its wall with the sharp spoon. An incision is made which will give free access to the interior of the abscess, so that outlying pockets or recesses may not be overlooked. After removal of the pus, the wall of the abscess is scraped with the Volkmann spoon or with Barker's flushing spoon, to get rid of the tuberculous tissue with which it is lined. In using the spoon, care must be taken that its sharp edge does not perforate the wall of a vein or other important structure. Any debris which may adhere to the walls is removed by rubbing with dry gauze. The oozing of blood is arrested by packing the cavity for a few minutes with gauze. After the packing is removed, iodoform powder is rubbed into the raw surface. The soft parts divided by the incision are sutured in layers so as to ensure primary union. If, on the other hand, there is fear of a mixed infection, especially in abscesses near the rectum or anus, it is safer to treat it by the open method, packing the cavity with iodoform worsted or bismuth gauze, which is renewed at intervals of a week or ten days as the cavity heals from the bottom.
Another method is to incise the abscess, cleanse the cavity with gauze, irrigate with Carrel-Dakin solution and pack with gauze smeared with the dilute non-toxic B.I.P.P. (bismuth and iodoform 2 parts, vaseline 12 parts, hard paraffin, sufficient to give the consistence of butter). The wound is closed with “bipped” silk sutures; one of these—the “waiting suture”—is left loose to permit of withdrawal of the gauze after forty-eight hours; the waiting suture is then tied, and delayed primary union is thus effected.
When the skin over the abscess is red, thin, and about to give way, as is frequently the case when the abscess is situated in the subcutaneous cellular tissue, any skin which is undermined and infected with tubercle should be removed with the scissors at the same time that the abscess is dealt with.
In abscesses treated by the open method, when the cavity has become lined with healthy granulations, it may be closed by secondary suture, or, if the granulating surface is flush with the skin, healing may be hastened by skin-grafting.
If the tuberculous abscess has burst and left a sinus, this is apt to persist because of the presence of tuberculous tissue in its wall, and of superadded pyogenic infection, or because it serves as an avenue for the escape of discharge from a focus of tubercle in a bone or a lymph gland.
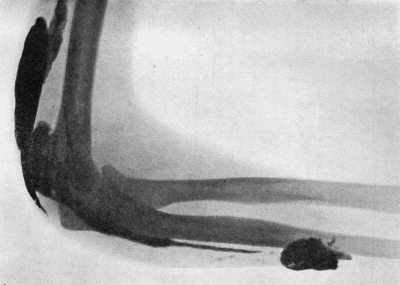
Fig. 35.—Tuberculous Sinus injected through its opening in the forearm with bismuth paste.
(Mr. Pirie Watson's case—Radiogram by Dr. Hope Fowler.)
The treatment varies with the conditions present, and must include measures directed to the lesion from which the sinus has originated. The extent and direction of any given sinus may be demonstrated by the use of the probe, or, more accurately, by injecting the sinus with a paste consisting of white vaseline containing 10 to 30 per cent. of bismuth subcarbonate, and following its track with the X-rays (Fig. 35).
It was found by Beck of Chicago that the injection of bismuth paste is frequently followed by healing of the sinus, and that, if one injection fails to bring about a cure, repeating the injection every second day may be successful. Some caution must be observed in this treatment, as symptoms of poisoning have been observed to follow its use. If they manifest themselves, an injection of warm olive oil should be given; the oil, left in for twelve hours or so, forms an emulsion with the bismuth, which can be withdrawn by aspiration. Iodoform suspended in glycerin may be employed in a similar manner. When these and other non-operative measures fail, and the whole track of the sinus is accessible, it should be laid open, scraped, and packed with bismuth or iodoform gauze until it heals from the bottom.
The tuberculous ulcer is described in the chapter on ulcers.