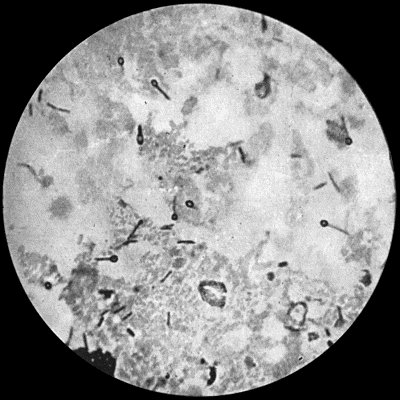
Fig. 26.—Bacillus of Tetanus from scraping of a wound of finger, × 1000 diam. Basic fuchsin stain.
Tetanus is a disease resulting from infection of a wound by a specific micro-organism, the bacillus tetani, and characterised by increased reflex excitability, hypertonus, and spasm of one or more groups of voluntary muscles.
Etiology and Morbid Anatomy.—The tetanus bacillus, which is a perfect anaërobe, is widely distributed in nature and can be isolated from garden earth, dung-heaps, and stable refuse. It is a slender rod-shaped bacillus, with a single large spore at one end giving it the shape of a drum-stick (Fig. 26). The spores, which are the active agents in producing tetanus, are highly resistant to chemical agents, retain their vitality in a dry condition, and even survive boiling for five minutes.
The organism does not readily establish itself in the human body, and seems to flourish best when it finds a nidus in necrotic tissue and is accompanied by aërobic organisms, which, by using up the oxygen in the tissues, provide for it a suitable environment. The presence of a foreign body in the wound seems to favour its action. The infection is for all practical purposes a local one, the symptoms of the disease being due to the toxins produced in the wound of infection acting upon the central nervous system.
The toxin acts principally on the nerve centres in the spinal medulla, to which it travels from the focus of infection by way of the nerve fibres supplying the voluntary muscles. Its first effect on the motor ganglia of the cord is to render them hypersensitive, so that they are excited by mild stimuli, which under ordinary conditions would produce no reaction. As the toxin accumulates the reflex arc is affected, with the result that when a stimulus reaches the ganglia a motor discharge takes place, which spreads by ascending and descending collaterals to the reflex apparatus of the whole cord. As the toxin spreads it causes both motor hyper-tonus and hyper-excitability, which accounts for the tonic contraction and the clonic spasms characteristic of tetanus.
Clinical Varieties of Tetanus.—Acute or Fulminating Tetanus.—This variety is characterised by the shortness of the incubation period, the rapidity of its progress, the severity of its symptoms, and its all but universally fatal issue in spite of treatment, death taking place in from one to four days. The characteristic symptoms may appear within three or four days of the infliction of the wound, but the incubation period may extend to three weeks, and the wound may be quite healed before the disease declares itself—delayed tetanus. Usually, however, the wound is inflamed and suppurating, with ragged and sloughy edges. A slight feverish attack may mark the onset of the tetanic condition, or the patient may feel perfectly well until the spasms begin. If careful observations be made, it may be found that the muscles in the immediate neighbourhood of the wound are the first to become contracted; but in the majority of instances the patient's first complaint is of pain and stiffness in the muscles of mastication, notably the masseter, so that he has difficulty in opening the mouth—hence the popular name “lock-jaw.” The muscles of expression soon share in the rigidity, and the face assumes a taut, mask-like aspect. The angles of the mouth may be retracted, producing a grinning expression known as the risus sardonicus.
The next muscles to become stiff and painful are those of the neck, especially the sterno-mastoid and trapezius. The patient is inclined to attribute the pain and stiffness to exposure to cold or rheumatism. At an early stage the diaphragm and the muscles of the anterior abdominal wall become contracted; later the muscles of the back and thorax are involved; and lastly those of the limbs. Although this is the typical order of involvement of the different groups of muscles, it is not always adhered to.
To this permanent tonic contraction of the muscles there are soon added clonic spasms. These spasms are at first slight and transient, with prolonged intervals between the attacks, but rapidly tend to become more frequent, more severe, and of longer duration, until eventually the patient simply passes out of one seizure into another.
The distribution of the spasms varies in different cases: in some it is confined to particular groups of muscles, such as those of the neck, back, abdominal walls, or limbs; in others all these groups are simultaneously involved.
When the muscles of the back become spasmodically contracted, the body is raised from the bed, sometimes to such an extent that the patient rests only on his heels and occiput—the position of opisthotonos. Lateral arching of the body from excessive action of the muscles on one side—pleurosthotonos—is not uncommon, the arching usually taking place towards the side on which the wound of infection exists. Less frequently the body is bent forward so that the knees and chin almost meet (emprosthotonos). Sometimes all the muscles simultaneously become rigid, so that the body assumes a statuesque attitude (orthotonos). When the thoracic muscles, including the diaphragm, are thrown into spasm, the patient experiences a distressing sensation as if he were gripped in a vice, and has extreme difficulty in getting breath. Between the attacks the limbs are kept rigidly extended. The clonic spasms may be so severe as to rupture muscles or even to fracture one of the long bones.
As time goes on, the clonic exacerbations become more and more frequent, and the slightest external stimulus, such as the feeling of the pulse, a whisper in the room, a noise in the street, a draught of cold air, the effort to swallow, a question addressed to the patient or his attempt to answer, is sufficient to determine an attack. The movements are so forcible and so continuous that the nurse has great difficulty in keeping the bedclothes on the patient, or even in keeping him in bed.
The general condition of the patient is pitiful in the extreme. He is fully conscious of the gravity of the disease, and his mind remains clear to the end. The suffering induced by the cramp-like spasms of the muscles keeps him in a constant state of fearful apprehension of the next seizure, and he is unable to sleep until he becomes utterly exhausted.
The temperature is moderately raised (100° to 102° F.), or may remain normal throughout. Shortly before death very high temperatures (110° F.) have been recorded, and it has been observed that the thermometer sometimes continues to rise after death, and may reach as high as 112° F. or more.
The pulse corresponds with the febrile condition. It is accelerated during the spasms, and may become exceedingly rapid and feeble before death, probably from paralysis of the vagus. Sudden death from cardiac paralysis or from cardiac spasm is not uncommon.
The respiration is affected in so far as the spasms of the respiratory muscles produce dyspnœa, and a feeling of impending suffocation which adds to the horrors of the disease.
One of the most constant symptoms is a copious perspiration, the patient being literally bathed in sweat. The urine is diminished in quantity, but as a rule is normal in composition; as in other acute infective conditions, albumen and blood may be present. Retention of urine may result from spasm of the urethral muscles, and necessitate the use of the catheter.
The fits may cease some time before death, or, on the other hand, death may occur during a paroxysm from fixation of the diaphragm and arrest of respiration.
Differential Diagnosis.—There is little difficulty, as a rule, in diagnosing a case of fulminating tetanus, but there are several conditions with which it may occasionally be confused. In strychnin poisoning, for example, the spasms come on immediately after the patient has taken a toxic dose of the drug; they are clonic in character, but the muscles are relaxed between the fits. If the dose is not lethal, the spasms soon cease. In hydrophobia a history of having been bitten by a rabid animal is usually forthcoming; the spasms, which are clonic in character, affect chiefly the muscles of respiration and deglutition, and pass off entirely in the intervals between attacks. Certain cases of hæmorrhage into the lateral ventricles of the brain also simulate tetanus, but an analysis of the symptoms will prevent errors in diagnosis. Cerebro-spinal meningitis and basal meningitis present certain superficial resemblances to tetanus, but there is no trismus, and the spasms chiefly affect the muscles of the neck and back. Hysteria and catalepsy may assume characters resembling those of tetanus, but there is little difficulty in distinguishing between these diseases. Lastly, in the tetany of children, or that following operations on the thyreoid gland, the spasms are of a jerking character, affect chiefly the hands and fingers, and yield to medicinal treatment.
Chronic Tetanus.—The difference between this and acute tetanus is mainly one of degree. Its incubation period is longer, it is more slow and insidious in its progress, and it never reaches the same degree of severity. Trismus is the most marked and constant form of spasm; and while the trunk muscles may be involved, those of respiration as a rule escape. Every additional day the patient lives adds to the probability of his ultimate recovery. When the disease does prove fatal, it is from exhaustion, and not from respiratory or cardiac spasm. The usual duration is from six to ten weeks.
Delayed Tetanus.—During the European War acute tetanus occasionally developed many weeks or even months after a patient had been injured, and when the original wound had completely healed. It usually followed some secondary operation, e.g., for the removal of a foreign body, or the breaking down of adhesions, which aroused latent organisms.
Local Tetanus.—This term is applied to a form of the disease in which the hypertonus and spasms are localised to the muscles in the vicinity of the wound. It usually occurs in patients who have had prophylactic injections of anti-tetanic serum, the toxins entering the blood being probably neutralised by the antibodies in circulation, while those passing along the motor nerves are unaffected.
When it occurs in the limbs, attention is usually directed to the fact by pain accompanying the spasms; the muscles are found to be hard and there are frequent twitchings of the limb. A characteristic reflex is present in the lower extremity, namely, extension of the foot and leg when the sole is tickled.
Cephalic Tetanus is another localised variety which follows injury in the distribution of the facial nerve. It is characterised by the occurrence on the same side as the injury, of facial spasm, rapidly followed by more or less complete paralysis of the muscles of expression, with unilateral trismus and difficulty in swallowing. Other cranial nerves, particularly the oculomotor and the hypoglossal, may also be implicated. A remarkable feature of this condition is that although the muscles are irresponsive to ordinary physiological stimuli, they are thrown into spasm by the abnormal impulses of tetanus.
Trismus.—This term is used to denote a form of tetanic spasm limited to the muscles of mastication. It is really a mild form of chronic tetanus, and the prognosis is favourable. It must not be confused with the fixation of the jaw sometimes associated with a wisdom-tooth gumboil, with tonsillitis, or with affections of the temporo-mandibular articulation.
Tetanus neonatorum is a form of tetanus occurring in infants of about a week old. Infection takes place through the umbilicus, and manifests itself clinically by spasms of the muscles of mastication. It is almost invariably fatal within a few days.
Prophylaxis.—Experience in the European War has established the fact that the routine injection of anti-tetanic serum to all patients with lacerated and contaminated wounds greatly reduces the frequency of tetanus. The sooner the serum is given after the injury, the more certain is its effect; within twenty-four hours 1500 units injected subcutaneously is sufficient for the initial dose; if a longer period has elapsed, 2000 to 3000 units should be given intra-muscularly, as this ensures more rapid absorption. A second injection is given a week after the first.
The wound must be purified in the usual way, and all instruments and appliances used for operations on tetanic patients must be immediately sterilised by prolonged boiling.
Treatment.—When tetanus has developed the main indications are to prevent the further production of toxins in the wound, and to neutralise those that have been absorbed into the nervous system. Thorough purification with antiseptics, excision of devitalised tissues, and drainage of the wound are first carried out. To arrest the absorption of toxins intra-muscular injections of 10,000 units of serum are given daily into the muscles of the affected limb, or directly into the nerve trunks leading from the focus of infection, in the hope of “blocking” the nerves with antitoxin and so preventing the passage of toxins towards the spinal cord.
To neutralise the toxins that have already reached the spinal cord, 5000 units should be injected intra-thecally daily for four or five days, the foot of the bed being raised to enable the serum to reach the upper parts of the cord.
The quantity of toxin circulating in the blood is so small as to be practically negligible, and the risk of anaphylactic shock attending intra-venous injection outweighs any benefit likely to follow this procedure.
Baccelli recommends the injection of 20 c.c. of a 1 in 100 solution of carbolic acid into the subcutaneous tissues every four hours during the period that the contractions persist. Opinions vary as to the efficiency of this treatment. The intra-thecal injection of 10 c.c. of a 15 per cent. solution of magnesium sulphate has proved beneficial in alleviating the severity of the spasms, but does not appear to have a curative effect.
To conserve the patient's strength by preventing or diminishing the severity of the spasms, he should be placed in a quiet room, and every form of disturbance avoided. Sedatives, such as bromides, paraldehyde, or opium, must be given in large doses. Chloral is perhaps the best, and the patient should rarely have less than 150 grains in twenty-four hours. When he is unable to swallow, it should be given by the rectum. The administration of chloroform is of value in conserving the strength of the patient, by abolishing the spasms, and enabling the attendants to administer nourishment or drugs either through a stomach tube or by the rectum. Extreme elevation of temperature is met by tepid sponging. It is necessary to use the catheter if retention of urine occurs.